|
Social Security Amendments of 1972: Summary
and Legislative History
by
Robert M. Ball
PRESIDENT NIXON'S SIGNATURE on H.R. 1, the Social Security Amendments
of 1972, brought to a close 3 years of consideration of and deliberations
on proposals to improve the social security program. What the President
called "landmark legislation" became Public law 92-603 on
October 30, 1972. Among its most significant and far-reaching provisions
are:
-Higher benefits for most people eligible for benefits as aged widows
and widowers
-For men reaching age 62 in the future, repeal of the provisions under
which a man the same age and with the same earnings as a woman generally
got a lower benefit than the woman worker and under which men needed
more social security credits to qualify for retirement benefits than
women did (the change will be accomplished over a 3-year period beginning
with 1973)
-Changes in the retirement test to assure that the more a beneficiary
works and earns, the more spendable income (social security benefits
plus earnings after taxes) he will have, and to raise from $1,680
to $2,100 the annual exempt amount of earnings with future automatic
adjustment to keep pace with increases in earnings levels
-A special minimum benefit for those who have worked in covered employment
for many years, but at low earnings
-Higher benefits for workers who do not get social security retirement
benefits before age 65 but continue to work past that age
-Improvements in disability insurance protection (including a reduction
in the waiting period for benefits and extension of childhood disability
benefits to persons disabled between ages 18 and 22) as well as improved
protection for a worker's dependents and survivors
-Extension of Medicare protection to disability insurance beneficiaries
who have been on the social security disability benefit rolls for
at least 2 years
-Extension of Medicare protection to persons under age 65 (those getting
monthly social security benefits, those not getting benefits who have
worked in covered employment long enough to be insured, and the wives
or husbands and children of such persons) if they need hemodialysis
treatment for chronic kidney disease or require a kidney transplant
-Changes in the Medicare program to improve its operating effectiveness.
The amendments also created a new Federal supplemental security income
program, effective January 1974, for the needy aged, blind, and disabled.
Administered by the Social Security Administration but financed out
of general revenues of the Federal Government, this program will replace
the present Federal-State programs of old-age assistance, aid to the
blind, and aid to the permanently and totally disabled. Federal payments
under this program will assure minimum income levels; States may supplement
the Federal payments to maintain existing payment levels where these
are higher.
Other major social security legislation was enacted in July 1972.
Those amendments (1) provided a 20-percent across-the-board increase
in social security benefits effective for September 1972; (2) included
provisions for keeping social security benefit amounts up to date
automatically in the future as the cost of living rises; and (3) increased
from $9,000 in 1972 to $10,800 in 1973 and to $12,000 in 1974 the
maximum amount of a worker's annual earnings that may be counted in
figuring his and his family's social security benefits (and on which
he pays social security contributions) and provided in addition for
keeping the amount up to date automatically in the future as average
wages rise, and a revised contribution rate schedule, which included
increases in the hospital insurance rates to restore the financial
soundness of that part of the program.
A detailed summary of all major provisions enacted in 1972 is given
later in this article.
Background and Legislative History
ACTION IN 1969
On September 25, 1969, the President sent to the Congress his recommendations
for social security legislation. They included:
(1) A 10-percent across-the-board increase in social security cash
benefits;
(2) automatic adjustment of social security benefits to future increases
in the cost of living;
(3) an increase in the annual exempt amount of earnings under the
retirement test from $1,680 to $1,800, with a corresponding increase
in the monthly measure of retirement, and a provision for $1-for-$2
withholding of benefits for all earnings in excess of $1,800 (instead
of withholding $1 for each $2 earned above $1,680 through $2,880 and
for each $1 of earnings above $2,880), and a provision for automatic
adjustment of the test to future earnings levels;
(4) an increase in the social security contribution and benefit base
from $7,800 to $9,000 for 1972 and 1973, with provision for subsequent
automatic increases to take account of future increases in earnings
levels;
(5) an increase from 82.5 percent to 100 percent of the spouse's benefit
for a widow or widower who begins receiving benefits at age 65 or
later, with the benefit amount graded down to 82.5 percent for a widow
or widower who takes benefits at age 62;
(6) non-contributory earnings credits (in addition to credit for contributory
coverage of basic pay) of $100 a month for military service from January
1957 through December 1967, similar to the credits previously provided
for service after 1967;
(7) extension of childhood disability benefits to people who become
disabled after age 18 and prior to age 22;
(8) determination of benefit amounts and insured status for men on
the same basis as that for women in the existing law--that is, over
a period equal to the number of years up to age 62 rather than up
to age 65; and
(9) changes in the contribution rate schedules for both cash benefits
and for hospital insurance.
On September 30, 1969, the minority leader of the House of Representatives,
Gerald R. Ford, introduced H.R. 14080, a bill containing the President's
recommendations for social security legislation. The bill was referred
to the Committee on Ways and Means of the House of Representatives
for consideration.
On October 15, the Ways and Means Committee began public hearings
on H.R. 14080 and H.R. 14173, which contained President Nixon's proposals
for reforming the Federal-State programs of public assistance. Secretary
of Health, Education, and Welfare Robert H. Finch appeared as the
Administration's first witness. In his testimony, Secretary Finch
announced that the Administration was forwarding to the Committee
that day for its consideration (along with the Medicare provisions
of H.R. 14080) a proposed bill the "Health Cost Effectiveness
Amendments of 1969," containing several provisions intended to
strengthen administrative controls over program payments, coordinating
health facility reimbursement with community planning efforts, and
experimenting with alternative methods of reimbursement that it was
hoped would be considered for inclusion in the social security bill,
The public hearings continued until November 13 and the Committee
went into executive sessions on November 19.
15-percent benefit increase enacted.-Early in December
it became clear that the Senate would attach several amendments to
the Social Security Act to a tax bill that seemed certain of enactment.
The Committee on Ways and Means unanimously ordered reported to the
House a bill, H.R. 15095, which had been introduced on December 4
by Committee Chairman Wilbur D. Mills and the ranking minority member
of the Committee, Representative John D. Byrnes. As reported, the
bill provided for a 15-percent increase in social security benefits,
effective for January 1970, removing the $105 limitation on wife's
and husband's insurance benefits which had been enacted by the previous
Congress, and increasing the allocation of contribution income to
the disability insurance trust fund. Because the old-age, survivors,
and disability insurance (OASDI) program had a substantial favorable
actuarial balance (1.16 percent of taxable payroll), the benefit increases
that were provided did not necessitate increases in either the contribution
rates or the contribution and benefit base. The House passed the bill
on December 15, 1969 by a vote of 398 to 0.
In the meantime H.R. 13270, the proposed Tax Reform Act of 1969, was
being debated and amended on the floor of the Senate. The amendments
that related to the social security program were to provide:
(1) A 15-percent across-the-board general increase in social security
benefits effective for January 1970;
(2) a minimum benefit of $100;
(3) an increase in the contribution and benefit base to $12,000 beginning
in 1973;
(4) elimination of the $105 limitation on wife's and husband's benefits;
(5) actuarially reduced benefits payable at age 60 for workers, wives,
husbands, widowers, and parents;
(6) a disregard of social security benefit increases for January and
February 1970 in determining eligibility for, and amount of, public
assistance; and
(7) a guarantee that all those receiving both aid to the aged, blind,
or disabled and social security benefits would receive a net increase
in income of at least $7.50 for months after March 1970.
The Tax Reform Act, with these amendments, was passed by the Senate
by a vote of 69 to 22. It was sent to a House-Senate conference committee
on December 11 to settle the differences between the two versions
of the bill. The conferees agreed upon:
(1) A 15-percent across-the-board general increase in social security
benefits effective for January 1970;
(2) elimination of the $105 limitation on wife's and husband's benefits;
(3) an increase in the allocation of contribution income to the disability
insurance trust fund;
(4) a disregard of social security benefit increases for January and
February 1970 in determining eligibility for, and amount of, public
assistance; and
(5) a guarantee that all people receiving aid to the aged, blind,
or disabled and also social security benefits for any month after
March 1970 and before July 1970 would receive a net increase in income
of at least $4 or, if less, the actual amount of the increase in their
social security benefits.
The report of the conference committee was agreed to by both the House
and the Senate on December 22. On December 30, the President signed
the Tax Reform Act of 1969 into law. It became Public Law 91-172.
ACTION IN 1970
In January the Ways and Means Committee resumed consideration of the
President's proposals. On May 11, a new bill, H.R. 17550, reflecting
the Committee's decisions, was introduced in the House by Chairman
Mills and Representative Byrnes.
The major social security proposals made by the President were included
in H.R. 17550 with several significant exceptions. In September 1969,
the President had recommended a 10-percent increase in cash benefits
effective for March 1970 and automatic adjustment of benefits in the
future. The Congress had subsequently enacted a 15-percent increase
in benefits effective for January 1970, and the Committee's bill provided
for an additional 5-percent increase in benefits to be effective for
January 1971. The bill did not include the President's proposal for
automatic adjustments of benefits (and of the contribution and benefit
base), though these proposals were later included in the bill before
it was passed by the House.
Under the Committee bill, the annual amount of earnings to be exempted
under the retirement test would have been increased from $1,680 to
$2,000, with $1 in benefits withheld for each $2 of earnings between
$2,000 and $3,200 and for each $1 of earnings above $3,200. The President
had recommended an annual exempt amount of $1,800, with $1 in benefits
to be withheld for each $2 of all annual earnings above $1,800 and
automatic adjustment of the exempt amount to keep pace with increases
in earnings levels.
The contribution rates approved by the Committee were in accord with
those recommended by the President but differed in detail from his.
The Committee also provided for significant changes in the financing
of the hospital insurance program, intended to restore it to a state
of acceptable actuarial balance.
H.R. 17550 included further changes in the cash benefits program,
in addition to those recommended by the President. Among these were
provisions for the payment of reduced benefits to dependent widowers,
at age 60, elimination of the support requirement as a condition for
benefits for divorced wives and widows, continuing child's benefits
beyond age 22 for certain full-time students, changes in the disability
insured status requirements for the blind, and a change in the workmen's
compensation offset for disability beneficiaries.
The provisions in the Committee bill dealing with the Medicare and
Medicaid programs reflected, for the most part, changes recommended
by the Department. In testimony before the Senate Finance Committee
in February, concerning that Committee's Staff Report on Medicare
and Medicaid, Under Secretary.John G. Veneman recommended a change
in the method of reimbursing institutional providers under Medicare
and the introduction of additional limitations on the recognition
of physicians' fee increases. These recommendations were embodied
in the Committee on Ways and Means version of H.R. 17550, under which
(1) the Secretary was directed to develop large-scale experiments
and demonstration projects to test various methods of making payments
to providers of services on a prospective, rather than retroactive,
cost basis and (2) recognition of increases in physician fee levels
were to be related to indexes reflecting changes in costs of practice
for physicians and in earnings levels.
As part of the Administration's proposals to stimulate the development
of health maintenance organizations, announced by Secretary Finch
in March 1970, an HMO option for Medicare beneficiaries was added
to the bill. Under the option, Medicare beneficiaries could choose
to receive their covered services only through an HMO. The organization
would be paid on a capitation basis instead of being reimbursed for
individual physician visits or hospital stays. The Committee's bill
also included a number of other changes designed to improve the operating
effectiveness of the Medicare program (as well as changes to improve
the operations of the Medicaid and maternal and child health programs).
On May 21, the House passed H.R. 17550 by a vote of 344 to 32, after
re-commitment to the Committee for amendments to provide for the automatic
adjustment of benefits, the contribution and benefit base, and the
retirement test exempt amount. These provisions had been included
in the Administration's proposals for improving the program but were
not included in the bill reported out by the Ways and Means Committee.
In adding the provision for automatic adjustment of the retirement
test, the House also extended the $1-for-$2 deduction provision so
that it would apply to all earnings above the $2,000 annual exempt
amount.
Following House passage, the bill was sent to the Senate for consideration
and was referred to the Senate Committee on Finance, which began public
hearings on June 17. During the summer of 1970, the Committee continued
to hold hearings on H.R. 17550 and it also held hearings on H.R. 16311,
the proposed Family Assistance Act of 1970, which had superseded H.R.
14173. In September the Committee began consideration of the two bills
in executive sessions.
These sessions lasted from September 29 to December 9, when the Committee
completed its deliberations and reported a revised version of H.R.
17550 to the Senate. Many of the provisions of the House-passed bill
were approved by the Committee on Finance, but a number of changes
were made and new provisions were added. In the cash benefits area,
the major modifications included:
(1) A 10-percent increase in social security benefits instead of the
5-percent increase in the House-passed bill;
(2) a $100 regular minimum benefit rather than the $67.20 minimum
resulting from the 5-percent increase in the House-passed bill ;
(3) a limitation on the increase in widow's and widower's benefits
so that benefits would not exceed the amount the deceased spouse would
be receiving if he were still alive (as could have occurred under
the House-passed provision) ;
(4) automatic increases in contribution rates and in the contribution
and benefit base, with the stipulation (not included in the House
bill) that automatic increases would only go into effect in the absence
of Congressional action changing social security benefit levels, contribution
rates, or the contribution and benefit base. Also, half of the cost
of each automatic benefit increase would be financed by an increase
in the contribution rates and the other half by an increase in the
contribution and benefit base. (Under the House bill rising wages
with automatic adjustment of the contribution and benefit base would
have provided adequate financing, without increases in the contribution
rates.);
(5) basing benefits for men on earnings up to age 62, rather than
on earnings up to age 65, only for those coming on the rolls in the
future, to be accomplished over a 3-year transition period (instead
of immediately, as in the House-passed provision and for those already
on the rolls as well as future beneficiaries);
(6) in place of the House-passed provision which eliminated the recency-of-work
requirement for disability insurance benefits to the blind, a much
more far-reaching provision, under which insurance benefits were provided
for a blind person with 6 quarters of coverage earned at any time,
regardless of his ability to work;
(7) extension of the House-passed provision improving childhood disability
benefits, by providing that a person who was entitled to childhood
disability benefits could become reentitled if he becomes disabled
within 7 years after his prior entitlement was terminated;
(8) reduction of the waiting period for disability benefits from 6
months to 4 months (not included in the House-passed bill); and
(9) a revised contribution rate schedule for cash benefits.
The Committee deleted provisions under which (1) election to receive
actuarially reduced benefits in one category would not be applicable
to certain benefits in other categories; (2) the support requirements
for benefits for divorced women would be eliminated; and (3) the ceiling
on income from combined workmen's compensation and social security
disability benefits would be raised from 80 percent to 100 percent
of the worker's average earnings.
Medicare provisions that were added by the Committee included:
(1) Establishment of a peer review system through the use of organizations
representing a substantial number of practicing physicians in local
areas to be called Professional Standards Review Organizations (PSRO's)
(these organizations would assume responsibility for comprehensive
and ongoing review of services provided under Medicare and Medicaid);
(2) establishment of an Office of Inspector General for Health Administration
within the Department of Health, Education, and Welfare having the
responsibility to review and audit Medicare and other health programs
on a continuing and comprehensive basis and the authority to suspend
any regulation, practice, or procedure employed in the administration
of such programs if he determines that the suspension will promote
efficiency and economy of administration or that the regulation, practice,
or procedure involved is contrary to or does not carry out the objectives
and purposes of applicable provisions of law;
(3) provisions for conforming requirements for participation under
Medicare and Medicaid of extended care facilities and skilled nursing
homes;
(4) broadening of penalty provisions relating to the making of a false
statement of representation of a material fact in any application
for Medicare payments to include the soliciting, offering, or acceptance
of kickbacks or bribes by providers of health care services;
(5) establishment of a Provider Reimbursement Appeals Board to resolve
disputes between providers and fiscal intermediaries concerning the
amount of reasonable cost reimbursement;
(6) coverage of services involving the manipulation of the spine by
licensed chiropractors under Medicare if the chiropractor meets certain
minimum standards established by the Secretary;
(7) requirement that the Secretary of HEW make reports of a provider's
significant deficiencies (such as staffing, fire, safety, and sanitation)
a matter of public record readily available at social security offices
if, after a reasonable lapse of time (not to exceed 90 days), such
deficiencies are not corrected;
(8) requirement that the Secretary of HEW develop and employ proficiency
examinations to determine whether health care personnel, not otherwise
meeting specific formal criteria included in Medicare regulations,
have sufficient professional competence to be considered qualified
personnel for Medicare purposes; and
(9) a revised contribution schedule for hospital insurance.
In addition, the Finance Committee added a provision which would have
established a program of catastrophic health insurance under the Social
Security Act for all persons under age 65 who are insured under social
security, their spouses and dependent children, as well as all persons
under age 65 who are entitled to retirement, survivors, or disability
benefits. The health services covered under the provision would have
been those covered under the Medicare program, and coverage would
have been available after family health care expenses exceeded certain
defined limits. The program would have been administered through regular
Medicare administrative procedures and subject to all utilization,
cost, quality, and administrative controls applicable to that program.
Coverage under the program would have been effective beginning January
1972.
Committee modifications of the House-passed bill included:
(1) Expansion of the authority for the Secretary to engage in prospective
reimbursement experiments and to conduct experiments with methods
of payment or reimbursement designed to increase efficiency and economy,
to include experiments with various types of outpatient treatment
centers, including mental health centers;
(2) a liberalization in the definition of extended care and a provision
for deemed coverage of extended care or home health services if required
medical certification and plan of treatment are submitted promptly
; and
(3) elimination of provision for part B coverage of up to $100 per
calendar year of physical therapy services furnished by a licensed
physical therapist in his office or in the patient's home under a
physician's plan.
H.R. 17550 as modified by the Senate Finance Committee also included
certain changes in the welfare programs for families and for adults.
Changes in the welfare programs had been passed by the House in H.R.
16311, which contained the Administration's proposals. That bill was
not acted on separately by the Finance Committee but was, essentially,
incorporated in its consideration of H.R. 17550. With respect to the
aged, blind, and disabled, H.R. 16311 provided a substantially new
Federal-State program under a new title XVI, combining the three categories
into one adult assistance program. The minimum monthly income level
was to have been the higher of $110 or the State's standard on the
date of enactment. Uniform definitions of blindness and disability
were to be applied, and for the blind and disabled there would have
been a mandatory disregard of $85 of earned income plus one-half of
the remainder; there would have been an optional earnings exclusion
for the aged of $60 per month plus one-half of additional earnings.
The resource limitations for all would have been $1,500, plus home,
personal effects, and incomeproducing property essential to support.
This new program would have prevented the States from imposing any
duration of residency requirement, and they could not have citizenship
requirements affecting United States citizens or aliens lawfully admitted
for permanent residence and residing continuously for 5 years, nor
could there be relative responsibility provisions other than for spouses
or parents.
Under the House bill, the Federal Government was to share the administrative
costs on a dollar-for-dollar basis and pay 90 percent of the first
$65 of average payments to recipients and 25 percent of the remainder,
up to a maximum to be set by the Secretary. Any State could have agreed
to have the Federal Government administer all or part of the program
and thereby have the administrative costs paid by the Federal Government.
The Senate Finance Committee version of H.R. 17550 provided for retaining
the separate programs of aid to the aged, blind, and disabled, but
with national minimum income standards of $130 for an individual and
$200 for a couple (with States required to increase their standards
by $10 for an individual and $15 for a couple so that in States already
having standards above $120 and $190 for an individual and a couple,
respectively, recipients would realize an increase in income in connection
with the social security benefit increase), uniform definitions of
blindness and disability, similar to the social security definitions,
a prohibition of liens against the property of the blind as a condition
of eligibility for aid to the blind, and a provision to assure that
all additional expenditures required by the bill with respect to aid
for the aged, blind, and disabled would be met without increasing
State costs.
The bill was reported to the Senate on December 11. During the final
2 weeks of the 91st Congress the Senate debated the bill. Floor amendments
were added to increase the annual exempt amount of earnings under
the retirement test from $2,000 (in the Committee bill) to $2,400,
to provide benefits for dependent grandchildren, and to raise the
ceiling on income from combined social security disability benefits
and workmen's compensation benefits from 80 percent to 100 percent
of a worker's average earnings prior to becoming disabled (the provision
had been deleted by the Committee). The Senate voted to recommit the
bill to delete title IV (the catastrophic health insurance program)
and title III (the Trade Act of 1970), as well as other provisions
of the bill. The bill was passed by a vote of 81 to 0 on December
29.
The Senate requested a conference and appointed conferees. However,
there was no conference and the bill died with adjournment, January
2, 1971. Chairman Mills indicated he would make social security legislation
the Ways and Means Committee's first order of business in the 92d
Congress.
In 1970, an amendment to the act to continue the suspension of duties
on manganese ore (P.L. 91-306) extended the pass-along of $4 of the
1970 social security benefit increase for recipients of aid to the
aged, blind, and disabled. As enacted in the Tax Reform Act of 1969,
the pass-along was effective only for the period April-June 1970.
P.L. 91-306 extended the provision through October 1970. In the closing
days of the 91st Congress, another bill was passed which further extended
the $1 pass-along provision. As passed by the House, the pass-along
provision would have become permanent, but a Senate amendment made
the extension effective only through December 1971. This bill was
enacted in January 1971 as P.L. 91-669.
ACTION IN 1971
When the 92d Congress convened, Chairman Mills and Representative
Byrnes jointly introduced H.R. 1, the social security provisions of
which were, for the most part, the same as those passed by the House
in H.R. 17550 in 1970. (In a few cases the provisions of H.R. 1 incorporated
changes made by the Senate in the House-passed version of H.R. 17550.)
H.R. 1 also included welfare reform provisions passed by the House
in a separate bill in 1970. The Ways and Means Committee held executive
sessions on H.R. 1 from February through May. No public hearings were
held since they had previously been held on essentially the same proposals.
10-percent benefit increase enacted.-In February and March
of 1971, the Congress was also considering H.R. 4690, a bill to increase
the public debt limit. During the debate the Senate added several
social security amendments to the bill. The House-Senate conference
committee, which met to resolve the differences, deleted two social
security provisions--those calling for a $100 minimum benefit and
for a $2,400 annual exempt amount under the retirement test--but accepted
the other social security changes which had been added by the Senate.
The President signed the bill into law on March 17. It became Public
Law 92-5.
The new law provided a 10-percent across-the-board increase in social
security benefits, including future maximum family benefits--the maximum
amount payable to a family based on one worker's earnings. Under earlier
benefit increases, maximum family benefits were increased only for
families whose benefits were limited to the maximum on the effective
date of the increase. In its report, the conference committee explained
that this new method of increasing maximum family benefits was intended
to "change the basic nature of the family maximum by making it
a percentage of the primary insurance amount rather than a percentage
of the worker's average monthly wage."
Under the change, families coming on the rolls after all increase
in benefits has been enacted will get the same benefits as those already
on the rolls.
The special monthly payments made to certain individuals aged 72 and
over who are not insured for regular social security cash benefits
were increased by only 5 percent. Both the 10-percent across-the-board
increase and the 5-percent increase in special age 72 payments were
effective retroactively to January 1971.
The social security contribution and benefit base was increased from
$7,800 to $9,000, beginning in 1972. In addition, the contribution
rate for the social security cash benefits program for 1976 and after
was increased from 5.0 percent each for employees and employers to
5.15 percent. There was no change in the contribution rate for the
self-employed.
1971 Advisory Council on Social Security. In March, the Advisory
Council on Social Security--a group composed, by law, of representatives
of organizations of employers and employees in equal numbers, and
representatives of the self-employed and the public, and including
many distinguished leaders in insurance, labor, business, and other
fields--issued its reports. The Council had been appointed by Secretary
Finch in 1969 and had conducted a comprehensive study of all aspects
of the social security program. Its recommendations for changes in
the social security cash benefits program included most of the major
changes relating to cash benefits that were contained in H.R. I and
major changes in financing policy, which will be described.
Further action on H.R. 1-In May, the Committee on Ways and
Means completed its consideration of H.R. 1 and sent the bill, as
amended by the Committee, to the House for its consideration.
As approved by the Committee, H.R. 1 called for a 5-percent, across-the-board
benefit increase, effective for June 1972, and an increase in the
contribution and benefit base to $10,200, beginning in 1972. It also
contained the major cash benefits and Medicare provisions that were
in H.R. 17550 in 1970--some as they were passed by the House, others
that were passed by the House but modified by the Senate, and still
others that were added to the House-passed version by the Senate.
The bill included compromise provisions for automatically adjusting
benefits to increases in prices and for automatically adjusting the
contribution and benefit base and the retirement test exempt amount
to increases in earnings levels; increased benefits for widows and
widowers, with benefits limited to the amount the worker would be
getting if he were alive; an age-62 computation point for men effective
over a 3-year transitional period; liberalization of the retirement
test; and the several health cost effectiveness amendments to the
Medicare program.
Several major provisions affecting cash benefits that were not in
the 1970 House-passed bill (H.R. 179550) were added by the Committee.
These included a special minimum benefit for people who work for 15
or more years under social security; additional dropout years for
long-term workers; increased benefits for workers who delay retirement
beyond age 65; computation of benefits for certain married couples
based on their combined earnings, and a reduction in the waiting period
for disability benefits from 6 months to 5 months.
The Committee's bill also included a number of new provisions in the
Medicare area. The most significant of these was the extension of
Medicare protection to the disabled. Other provisions, not in the
House-passed bill in 1970, included: a restriction on increases in
the amount of the supplementary medical insurance premium so that
each increase would be limited to the percentage by which benefits
had been increased across-the-board since the premium was last increased;
automatic enrollment (subject to individual opting out) for supplementary
insurance for people entitled to hospital insurance; an increase in
the supplementary medical insurance deductible from $50 to $60 per
year; an increase in the lifetime reserve under hospital insurance
from 60 to 120 days: and coinsurance equal to one-eighth of the inpatient
hospital deductible for each day of inpatient hospital coverage during
a benefit period beginning with the 31st day and through the 60th
day.
In order to pay the additional cost of the changes made by the Committee
in the cash benefits and hospital insurance programs and to restore
the actuarial soundness of the hospital insurance program, a new schedule
of contribution rates was provided and the contribution and benefit
base was raised.
H.R. 1 also contained provisions for far-reaching reforms in the Nation's
public assistance programs. Three new Federal welfare programs incorporating
the President's plans for welfare reform were included. In line with
Administration recommendations, one was to be a Federal adult assistance
program to replace the existing Federal-State programs of aid to the
aged, blind, and permanently and totally disabled. Two new Federal
programs were to replace the program of aid to families with dependent
children to provide assistance for the working poor.
The provisions for a Federal adult assistance program differed significantly
from the adult assistance provisions of H.R. 16311 (passed by the
House in 1970) and H.R. 1 as it was introduced. Under the Committee's
bill, a new title XX of the Social Security Act would establish a
totally Federal program to replace the Federal-State programs of old-age
assistance, aid to the blind, and aid to the permanently and totally
disabled, beginning July 1, 1972; provisions were included, however,
for States to supplement the Federal payments with the objective of
continuing higher payment levels where they existed. The Federal program
and the State supplement, if the State so elected, would be administered
by the Social Security Administration.
The Committee bill provided for full monthly payments (assuming no
other income) of $130 for an individual for fiscal year 1973, $140
for fiscal year 1974, and $150 thereafter; for a couple, $195 for
fiscal year 1973, and $200 thereafter. Aged, blind, and disabled persons
would be eligible if their income (except for certain exclusions)
did not exceed the full benefit amount, and their resources did not
exceed $1,500. A home, household goods, personal effects, and property
essential to self-support generally would not be counted as resources.
The principal exclusion of income from consideration in determining
eligibility and payment amounts applied to earnings: the first $85
of earnings per month and one-half above $85 for the blind and disabled
(plus work expenses for the blind), and the first $60 of earnings
per month and one-third above $60 for the aged.
Definitions of disability and blindness under the adult assistance
provisions were generally the same as under the social security (title
II) provisions. Disabled and blind recipients would be referred to
State agencies for consideration for vocational rehabilitation services;
refusal, without good cause, to accept offered vocational rehabilitation
services would mean ineligibility for assistance payments.
States choosing to provide their own supplements to the Federal payments
could have the Federal Government administer the supplements, with
the Federal Government paying full administrative costs. States also
were provided with a guarantee that if they supplemented the Federal
payments, to the extent that the Federal payments and a State's supplementary
payments to recipients did not exceed the payment levels in effect
under public assistance programs in the State in January 1971, their
costs for the payments would not exceed their total expenditures for
all public assistance payments in calendar 1971; the Federal Government
would assume the additional cost.
Following the Ways and Means Committee's action on H.R. 1, President
Nixon endorsed the bill, calling it "the single most significant
piece of social legislation to be considered by the Congress in decades."
In his statement, the President said:
"The House Ways and Means Committee has taken a momentous
step in approving H.R. 1. This bill, with its important symbolic designation
as the first order of business of the 92d Congress, represents an
important landmark in the history of both social security and public
welfare reform. As reported by the Committee, under the responsible
leadership of Chairman Wilbur Mills and Congressman John Byrnes, this
bill represents the finest kind of cooperation between this administration
and the Congress."
The President also said, however, that there were areas in the bill
that could be improved In particular, he continued to urge inclusion
of his proposal to eliminate the supplementary medical insurance premium
and to finance the supplementary medical insurance program (as hospital
insurance is financed) through employer-employee contributions made
during the working years, rather than from reduced retirement incomes.
On June 22, H.R. 1 was passed by a House vote of 288 to 132 and sent
to the Senate for consideration. The Senate Committee on Finance held
public hearings in July and August, but no further action was taken
until 1972.
Late in 1971, the Congress passed and the President signed into law
H.R. 10604, which contained a minor social security amendment. It
permitted the payment of the social security lump-sum death payment
in cases where the body of an insured worker is not available for
burial and the worker had no spouse who was living with him at the
time of his death. (The law already provided that the spouse of a
worker who was living with him before his death could get the lump-sum
death payment whether or not the body was available for burial.)
Under the change, where no body is available for burial, the provisions
previously applicable where a body was available will apply; that
is, the lump-sum death benefit is paid to any equitably entitled person,
or persons, to the extent and in proportion to the expenses each person
incurred in connection with the death of the insured worker. The expenses
can include a memorial service, a memorial marker, a site for the
marker, or other expenses customarily incurred in connection with
a death. The amendment was effective for deaths occurring after 1970.
The bill extended until the end of 1972 the $4 pass-along provision
that was first enacted in 1969 to guarantee recipients of aid to the
aged, blind, and disabled, who also receive social security benefits,
an increase in income as a result of the social security benefit increase
effective for January 1970. Had the amendment not been passed, the
pass-along provision would have expired at the end of 1971.
ACTION IN 1972
Further public hearings on H.R. 1 were held by the Senate Finance
Committee in January and February of 1972, and the bill was then considered
by the Committee in executive sessions through June. While these sessions
were going on, interest in providing another substantial benefit increase
was growing. On February 23, 1972, Chairman Mills introduced a bill,
H.R. 133207 calling for a 20-percent increase in social security benefits,
an increase in the contribution and benefit base to $10,200 in 1972
and to $12,000 in 1973, and automatic increases in benefits and the
contribution and benefit base.
The contribution rate schedule in H.R. 13320 was based on financing
recommendations that had been made by the 1971 Advisory Council on
Social Security in its reports that year and that had subsequently
been endorsed by the boards of trustees of the social security trust
funds and by the Nixon administration. Under the practice usually
followed in the past, when a schedule of social security contribution
rates was enacted, it was generally designed to provide income slightly
in excess of expenditures for the first few years after enactment
and sufficient income to build up large trust funds in later years.
Interest earned by investing these accumulated funds would provide
a significant amount of income that would help to support the program
in future years. The Advisory Council's recommendation reflected in
H.R. 13320 was that the law should include contribution rates sufficient
to finance all benefit costs (assuming that benefits are increased
as the cost of living increases) fund administrative expenses of the
program, but that would keep the trust funds at a contingency-reserve
level--a level approximately equal to one year's expenditures.
In this regard the Council's recommendation was in basic accord with
the practice followed in financing social security for many years.
Over the years, when Congress has provided for changes in the social
security program, it has generally postponed the effective date of
the high contribution rates under which the large trust funds would
accumulate and provided new current rates at levels necessary to meet
program costs and allow for relatively small annual increases in the
trust funds. The Council's recommendation, then, reflected the way
the program had, in fact, been financed over the past 20 years.
The Council also recommended, and H.R. 130320 reflected, a change
in the assumptions used in making the cost estimates on which contribution
rates are based. In the past, cost estimates were based on the assumption
that wages and benefits would remain level. When wages did in fact
rise, the actual income to the program was greater than the income
shown in the estimates. As a result, the program was over-financed;
the contribution rates in the law were higher than were necessary
to meet the cost of the benefits payable under the program. The Council
recommended that the cost estimates used to determine contribution
rates should be based on the assumption that wages and benefits will
continue to rise in the future as they have in the past. Thus, the
financing recommendations of the Advisory Council made it possible
to finance the existing social security benefits with lower contribution
rates for the next 40 years than were then in the law.
On June 30, 1972, during its consideration of H.R. 15390, a bill which
provided for an extension of the public debt limitation, the Senate
added an amendment, introduced on June 28 by Senator Frank Church,
which was substantially the same as the Mills bill. (The 20-percent
benefit increase was to be effective for September 1972, instead of
June, as under the Mills bill, and the contribution and benefit base
was to be increased to $10,800 in 1973, and to $12,000 in 1974, with
automatic adjustments thereafter.) Both the Church amendment and the
Mills bill provided for financing the cost of automatic benefit increases
from increases in the contribution and benefit base, rather than financing
half the cost from increases in the contribution rates and the other
half from increases in the base as the Senate Committee on Finance
had recommended earlier.
The amendment also provided for a new contribution rate schedule based
on the financing recommendations of the Advisory Council, as had the
Mills bill. In addition, it corrected, through revised hospital insurance
contribution rates, the underfinancing of the hospital insurance program
and put that program on a financially sound basis.
H.R. 15390, with these social security amendments was passed by both
the Senate and the House on June 30, and on July 1 President Nixon
signed the bill into law. It became Public Law 92-336.
In September, the Senate Finance Committee again turned its attention
to H.R. 1 and on September 26 completed its deliberations and reported
the bill to the Senate. A number of changes in the House-passed bill
were made by the Committee. Major changes in the social security cash
benefits program included:
(1) Provision for a special minimum benefit of as much as $200 a month
for a person who had been in covered employment for 30 years, instead
of $150 a month;
(2) making the delayed retirement increment effective retrospectively;
(3) providing a $2,400 annual exempt amount under the retirement test;
and
(4) reducing the waiting period for disability benefits from 6 months
to 4 months (instead of 5 months as in the House provision).
The Committee added a number of new provisions, including one which
would have provided for the payment of benefits for certain aged dependent
sisters and disabled dependent brothers and sisters. It deleted the
provisions relating to actuarially reduced benefits in cases where
the beneficiary is eligible for benefits in more than one category,
computation of benefits on the basis of combined earnings of a married
couple, and dropping of additional years of low earnings from the
computation of benefits. In view of the fact that a 20-percent benefit
increase had just been enacted, the bill reported by the Committee
did not contain a general benefit increase.
With respect to Medicare, the Committee made substantial changes and
additions to the House passed bill. Again included were the amendments,
added earlier by the Senate to H.R. 17550, that related to Professional
Standards Review Organizations, an Inspector General for Health Administration,
disclosure of information concerning provider deficiencies, and coverage
of services of chiropractors. Substantive changes in the House-passed
version:
(1) Expanded the Secretary's experimental authority to include experiments
with payment for various forms of care (not currently covered under
Medicare) as alternatives to covered care, particularly the services
of physicians' assistants and additional types of institutional and
home care;
(2) eliminated provisions which would have (a) raised the part B annual
deductible from $50 to $60 and (b) covered services of independently
practicing physical therapists;
(3) eliminated the addition of coinsurance for the 31st through the
60th day of an inpatient hospital stay and an increased lifetime reserve
and substituted a provision reducing the lifetime reserve coinsurance
from one-half to one-fourth of the inpatient hospital deductible;
and
(4) changed the method of reimbursement of health maintenance organizations
to provide for sharing between the Government and an established HMO
of any savings achieved under the costs of non-HMO beneficiaries,
and recognized a second category of "newly established"
HMO's which would have prospective reimbursement payments retroactively
adjusted to reflect actual cost (the House bill authorized payment
on a capitation basis not to exceed 95 percent of the cost of Medicare
benefits had beneficiaries not been enrolled with an HMO).
Additions made by the Finance Committee included:
(1) Coverage of certain maintenance prescription drugs used in treatment
of most common chronic diseases of the elderly, with $1 co-payment
per prescription;
(2) extension of Medicare protection, on an optional basis, at cost
($33 monthly for part A and $11.60 monthly for part B) to spouses,
aged 60-64, of Medicare beneficiaries; to others aged 60-64 who are
entitled to retirement, dependents, or survivors benefits under the
social security or railroad retirement programs; and to disability
beneficiaries aged 60-64 not otherwise eligible for Medicare because
they have not been entitled to cash disability benefits for 24 months
(the House bill extended Medicare to uninsured persons 65 and over
on a voluntary, premium-financed basis);
(3) termination of the Medical Assistance Advisory Council and consolidation
of its functions with that of the Health Insurance Benefits Advisory
Council, as advisory body to the Secretary on matters of general Medicare
and Medicaid policy;
(4) provisions which would conform Medicare and Medicaid requirements
and procedures with respect to skilled nursing facilities (formerly
called ECF's under Medicare) and level of care requirements for reimbursement
of care received in such facilities (including a broadening of Medicare's
extended care definition to include certain rehabilitation care);
(5) requirement that the Secretary disclose certain information concerning
performance of State agencies, fiscal intermediaries, and carriers;
(6) program for validating, for Medicare purposes, accreditations
by the Joint Commission on Accreditations of Hospitals; and
(7) waiver of Medicare's 14-day transfer requirement for extended
care benefits in certain situations involving non-availability of
beds or unavoidable delay in start of a skilled care regimen.
The Senate Committee also made a number of substantial changes in
the welfare reform provisions of the bill. After previously (in June
of 1972) having made a tentative decision to abandon federalization
of adult assistance in favor of continuing State and local administration
of the existing programs of aid to the aged, blind, and disabled,
modified to set a Federal guaranteed minimum income level, the Senate
Finance Committee decided to include in its bill a Federal program
structured like that provided for by the House. Details of the Federal
program differed in certain significant respects from those in the
House bill. The Finance Committee provided for a new title XVI Federal
program of supplemental security income assuring aged, blind, and
disabled people of income of at least $130 a month for an individual
and $195 a month for a couple. The limit on assets of an eligible
individual or couple was set at $2,500, compared with $1,500 under
the House bill. It also called for an exclusion of $50 of any income,
which in the majority of cases would mean that $50 of social security
benefits would not count as income. The earned income exclusions were
set at $85 per month plus one-half of the rest for all three categories,
that is, aged, blind, and disabled. Those disabled under age 18 would
not have been eligible as they would have been under the House bill.
Disabled persons who were drug addicts or alcoholics were excluded
from eligibility for supplemental security income, but the bill established
a new program (title XV) to provide treatment and, if necessary, maintenance
payments for addicts and alcoholics who qualified under the new title
XV provisions.
The supplemental security income provisions were not made applicable
to Puerto Rico, Guam, and the Virgin Islands; the present Federal-State
programs were to remain in effect in those areas.
Debate on the bill began in the Senate on September 26 and continued
until October 6. A number of amendments were offered from the floor
and several were adopted. These included reduced benefits at age 60
for workers, wives, husbands, and parents, and at age 55 for widows;
an increase to $3,000 in the annual exempt amount of earnings under
the retirement test, with a corresponding change in the monthly measure;
Medicare coverage for most persons under age 65 suffering from chronic
kidney disease; elimination of the part B coinsurance payment for
home health services under Medicare; and coverage under Medicare for
coal miners entitled to black lung benefits.
On October 6, the bill passed the Senate by a vote of 68 to 5. The
Senate requested a conference with the House, and a committee was
appointed. The conferees met on October 10, and by October 14 they
had completed their work and submitted a report. Most of the welfare
provisions of the bill, except those relating to the new Federal adult
assistance program, as well as most of the changes in the bill, that
were added on the floor of the Senate, were dropped.
In the Medicare area, the conferees dropped the provisions relating
to the coverage of drugs, the creation of an Office of Inspector General,
coverage of miners on entitlement to black lung benefits, and coverage
for the uninsured aged 60-64. They agreed not to change the part A
coinsurance provisions or to increase the lifetime reserve days. The
conference committee compromises were agreed to by the House on October
17 by a vote of 305 to 1, and on the same day by the Senate by a vote
of 61 to 0. On October 30, 1972, H.R. 1 was signed into law by the
President and became Public Law 92-603.
Major Provisions of 1972 Social Security
Legislation
PUBLIC LAW 92-336
On July 1, 1972, President Nixon signed Public
Law 92-336, a bill to extend the public debt limit. The legislation
also contained amendment to the Social Security Act, raising the
amount of monthly cash benefits and revising several financing provisions.
Increase in Benefits
A 20-percent increase across the board was
provided for monthly cash benefits, including the special monthly
payments to certain individuals aged 72 and over who are not insured
for regular monthly benefits. The amendments also provided for automatic
increases in benefits as prices rise in the future. The first automatic
increase will be possible in 1975. The procedure in the law for
such increases is as follows:
In 1974 and every calendar year thereafter
(except in a calendar year in which a general benefit increase is
enacted or becomes effective), it will be determined if a "cost-of
-living" increase in cash benefits shall be established. For
the first determination, the arithmetical mean of the Consumer Price
Index (CPI) prepared by the Department of Labor for April, May,
and June of 1974 will be divided by the arithmetical mean of the
CPI for July, August, and September 1972. If such quotient (rounded
to the nearest one-half of 1 percent) is greater than or equal to
3 percent, then a "cost-of-living" increase in benefits
will be established in 1974 and the level of benefits will be increased
by the same percentage, effective January 1, 1975. If the contribution
and benefit base is raised at the same time (see below), the benefit
formula will provide an additional 20 percent on average monthly
earnings above the previous monthly contribution and benefit base.
In subsequent years, the same procedure will
be followed except that the arithmetical mean of the CPI for April,
May, and June in the year of the computation will be divided by
the latest of (a) the arithmetical mean of the CPI for April, May,
and June of the year in which the last effective "cost-of -living"
increase was established or (b) the mean of the 3 months of the
quarter in which the effective month of the last general benefit
increase occurred (July-September 1972, if that is the latest such
quarter). When a "cost-of-living" increase is established,
the new benefits become effective on January 1 of the following
year.
The bill also included a revised tax rate
schedule that included increases in the hospital insurance rates
to restore the financial soundness of that part of the program.
Financing
A revised contribution rate schedule was
enacted (and later superseded by the schedule in the October amendments),
with rates as shown in the table . . . under the heading "old
law." The earnings base for contribution and benefit purposes
was also revised--from $9,000 in 1972 to $10,800 in 1973 and to
$12,000 in 1974. The base is to be raised automatically
in the future as wages rise, under the following procedure:
Whenever an automatic adjustment in monthly
cash benefits is made, a determination will also be made as to whether
an adjustment in the maximum amount of annual earnings that will
be taxed and credited toward benefits is required. The determination
is made by multiplying the contribution and benefit base in effect
in the year of determination by the ratio of the average taxable
wages (under the social security program) of all employees, as reported
in the first calendar quarter of the year of determination, to the
average taxable wages of all employees as reported for the latest
of (a) the first calendar quarter of 1973 or (b) the first calendar
quarter of the year in which the last automatic determination resulted
in a base increase or of the year in which a legislative increase
in the base was enacted. The product, rounded to the nearest multiple
of $300, will be the amount of the contribution and benefit base,
effective with respect to remuneration paid after the year of determination.
In no case, however, will the base be reduced to an amount lower
than the base in the year of determination.
PUBLIC LAW 92-603
Cash Benefits
Increase in widow's and widower's benefits.
A widow (or widower) who first becomes entitled to benefits at or
after age 65 receives a benefit equal to 100 percent of her deceased
husband's primary insurance amount if he did not receive reduced
benefits before his death. If he did receive reduced benefits, the
widow's benefit can be no more than the amount her husband would
be receiving if he were still alive. (A widow
who becomes entitled to benefits at or after age 62 receives
no less than 82.5 percent of her husband's primary insurance amount.)
Benefits for widows (or widowers) who become entitled between ages
62 and 65 are reduced to take account of the longer period over
which they are paid, just as widow's benefits are reduced, under
the previous law, between ages 60 and 62.
Age-62 computation point for men.-For
men who reach age 62 in the future, benefits will be based on average
monthly earnings figured up to age 62, as is now the case for women.
The change is to be accomplished in three steps: A man who reaches
age 62 in 1973 will have his average earnings figured over a period
1 year shorter than under the old law; a man who reaches age 62
in 1974 will have his earnings figured over a period 2 years shorter
than under previous law. For men reaching age 62 in 1975 or later,
the computation period will end at age 62 (3 years less than previously).
Similar changes are made in the insured-status requirements.
Liberalization and automatic adjustment
of the earnings test.-The annual exempt amount of earnings
is increased from $1,680 to $2,100. The amount of wages
an individual may earn in a month and still receive full benefits
for the month is raised from $140 to $175. Benefits are reduced
by $1 for each $2 of all earnings above $2,100. At no point
is $1 in benefits withheld for each $1 of earnings, as had been
the case for earnings above $2,880. The annual exempt amount in
the retirement test and the monthly test will be adjusted automatically
in the future to reflect rises in the general earnings levels, according
to the following procedure in the law:
A determination as to whether an adjustment
of the earnings test is required will be made in the year a "cost-of-living"
increase is established. The determination is made by multiplying
the exempt monthly amount that is effective with respect to months
in the year of determination by the ratio of the average taxable
wages of all employees, as reported in the first calendar quarter
of the year of determination, to the average taxable wages of all
employees as reported for the latest of (a) the first calendar quarter
of 1973 or (b) the first calendar quarter of the year in which the
last automatic determination resulted in an increase in the base
or of the year in which a legislative increase in the base was enacted.
The product, rounded to the nearest multiple
of $10, will be the new exempt monthly amount effective for the
taxable year beginning after the year of determination (unless Congress
has enacted an increase in the exempt amount in the year of determination).
In no case, however, will the new exempt amount be reduced to an
amount lower than the exempt amount in the year of determination.
In the year in which a person attains age
72, his earnings in and after the month of attainment of age 72
will not be included in determining his total earnings for the year.
(Before the amendment, they were included.) These provisions are
effective for taxable years ending after 1972.
Delayed retirement credit.-The average
benefit of a worker who does not take a reduced benefit is increased
by 1 percent for each year (1/12 of 1 percent for each month) after
1970 for which the worker between ages 65 and 72 did not receive
benefits because of earnings from work. No increased benefit will
be paid under this provision to the worker's dependents or survivors.
Special minimum primary insurance amount.
A special minimum benefit equal to $8.50 multiplied by a worker's
years of coverage in excess of 10 years, up to a maximum of 30 years,
is provided. The highest minimum benefit under this provision is
$170 a month for an individual ($255 for a couple) with 30 or more
years of coverage. A special minimum is thus payable to those who
worked for many years at low earnings under the social security
program. The special minimum will be paid as an alternative to the
regular benefit when a higher benefit results. If an increase is
provided under the automatic benefit increase provision in the law,
this special minimum will not, however, be raised.
Reduced benefits for widowers
at age 60. Non-disabled widowers, like widows, may elect to
receive reduced benefits at age 60.
Changes in disability provisions.-Several
changes have been made that relate to the disability program:
1. The waiting period throughout which a
person must be disabled before disability benefits can begin is
reduced from 6 months to 5 months. The first benefit is payable
for the sixth month of disability.
2. A blind person will be insured for disability
insurance benefits if he is fully insured-that is, if he has as
many quarters of coverage as the number of calendar years elapsing
after the year he reached age 21 (or 1950, if later) and
up to the year in which he became disabled. He no longer has to
meet the requirement of recent covered work (generally 20 quarters
of coverage in the period of 40 calendar quarters preceding disablement).
3. Childhood disability benefits are extended
to the disabled adult son or daughter of an insured deceased parent
or a parent eligible for old-age or disability insurance benefits
if the son or daughter became totally disabled after age 18 but
before age 22. Previously, benefits were limited to those disabled
before age 18. In addition, a person can now become re-entitled
to childhood disability benefits if he again becomes disabled within
7 years after his earlier entitlement to such benefits was terminated.
4. The amendments modify the provisions under
which social security disability benefits are reduced where workmen's
compensation is also payable. Previously, social security disability
benefits had been reduced if the combined payments from both programs
exceeded 80 percent of the worker's average current earnings before
disablement; average current earnings for this purpose were computed
on two different bases and the larger amount was used. The new provision
adds a third alternative base under which a worker's average current
earnings can be based on a single year of his highest earnings in
a period consisting of the year of disablement and the 5 preceding
years.
5. The application requirement for disability
insurance benefits (and dependents' benefits based on the worker's
entitlement to disability benefits) will be met if the application
is filed within 3 months after the disabled worker's death or within
3 months after enactment of the provision. (Previously, an application
had to be filed while the disabled worker was alive, either by the
disabled worker or, if he was unable to file, by another person
on his behalf.) This new provision applies with respect to deaths
occurring after 1969.
6. The amendments authorize an increase in
the amount of social security trust fund money that can be used
to pay the costs of rehabilitation services for social security
disability beneficiaries. The amount is increased from 1 percent
of the previous year s disability benefits under the old law, to
1.25 percent for fiscal year 1973 and to 1.5 percent for fiscal
year 1974 and thereafter.
Changes in eligibility requirements.
-The amendments include the following revisions relating
to eligibility:
1. The law no longer requires that to qualify
for benefits as a divorced wife, divorced widow, or surviving divorced
mother, a woman must show that a court order in effect provided
for substantial contributions to the woman's support by the former
husband, that she received substantial contributions from her former
husband, pursuant to a written agreement, or that she received half
her support from her former husband.
2. For a child who is attending school full
time when he reaches age 22, benefit payments will continue through
the end of the semester or quarter in which he reaches that age
if he has not received or completed the requirements for a bachelor's
degree from a college or university. If the educational institution
in which he is enrolled is not operated on a semester or quarter
system, benefits continue until the month following the completion
of the course in which he is enrolled or 2 calendar months have
elapsed after the month in which he reaches age 22, whichever occurs
first.
3. For children adopted by old-age and disability
insurance beneficiaries, the differences in eligibility requirements
for entitlement to child's benefits are repealed and new uniform
requirements for both cases are provided. Now, a child who is adopted
by a worker getting retirement or disability benefits, regardless
of when the adoption occurs, may get benefits if (1) the adoption
was decreed by a court of competent jurisdiction within the United
States; (2) the child was living with and receiving at least half
his support from the worker for at least 1 year before the worker
became entitled to retirement or disability benefits; and (3) the
child was under age 18 when he began to live with the worker. A
child born in the 1-year period during which he would otherwise
be required to have been living with and receiving at least half
his support from the retired or disabled beneficiary is deemed
to meet the living-with and support requirements if he
was living with the beneficiary in the United States and receiving
at least half his support from the beneficiary for substantially
all of the period occurring after his birth.)
This provision is effective with respect
to benefits payable for January 1968 and thereafter if an application
for benefits is filed within 6 months after the month of enactment;
otherwise, it is effective with respect to benefits payable for
the month of enactment and after.
4. Child's insurance benefits are provided
for a grandchild of a worker or of his spouse if (1) the child was
living with and receiving at least half his support from the worker
for the year immediately before the worker became disabled or entitled
to old-age or disability benefits or died; (2) the child began living
with the worker before he attained age 18; and (3) at the time the
worker became disabled or entitled or died (a) the child's natural
or adopting parents or stepparents were disabled or were not alive
or (b) the child was adopted by the worker or by the workers surviving
spouse after the Worker's death and the child's natural or adopting
parent or stepparent was not living in the worker's household and
making regular contributions toward the child's support at the time
the worker died. (A child born in the 1-year period during which
he would otherwise be required to have been living with and receiving
at least half his support from the grandparent is deemed to meet
the requirement if he was living with the grandparent in the United
States and receiving at least half his support from the grandparent
for substantially all of the period occurring after his birth.)
5. Effective on enactment, the amendments
repeal the provisions that required the termination of child's insurance
benefits if the child was adopted by someone other than (1) his
natural parent, (2) his natural parent's spouse jointly with the
natural parent, (3) the worker-a stepparent, for example--on whose
earnings the child was getting benefits, or (4) a stepparent, grandparent,
aunt, uncle, brother, or sister after the death of the worker on
whose earnings the child is getting benefits. A child whose entitlement
to benefits was terminated because of the earlier provision and
who would otherwise still be entitled may, on filing an application,
become re-entitled to benefits effective with the month of enactment
of the amendments.
6. The 3-month duration-of-relationship requirement
in the old law is repealed for cases of accidental death or death
in the line of duty as a member of a uniformed service on active
duty. Retained, however, is the prohibition against the payment
of benefits in cases where the relationship does not last 9 months
because of such deaths, if the Secretary of Health, Education, and
Welfare determines that at the time of the marriage of the deceased
individual he could not have reasonably been expected to live for
9 months. Also waived is the duration-of-relationship requirement
for entitlement to benefits as a worker's widow, widower, or stepchild
when the worker and his spouse were previously married, divorced,
and then remarried, the relationship existed at the time of the
worker's death, and the duration-of-relationship requirement would
have been met if the worker had died on the date he was divorced
from his spouse.
Wage credits for Members of the Uniformed Services.- Non-contributory
wage credits are provided, in addition to contributory credits for
basic pay, for military service during the period January 1957 (when
military service was first covered) through December 1967. (Previously,
such credits had been provided for military service beginning January
1968.) Wage credits will uniformly be $300 for each quarter in which
the serviceman receives military pay--rather than $100, $200, or
$300, depending on the amount of covered military pay in the quarter,
under the old provision. The new provision is effective for monthly
benefits after December 1972.
Members of religious orders taking a
vow of poverty. -Effective on enactment, the amendments extend
coverage to members of a religious order who have taken a vow of
poverty (with respect to services performed in the exercise of duties
required by the order) as employees of the order, if the order makes
an irrevocable election of coverage for its entire active membership
and for its lay employees. Wages for social security purposes will
be the fair market value of any board, lodging, clothing, and other
perquisites furnished to the member (but not less than $100 a month).
Each order can elect up to 5 years of retroactive coverage for persons
who were active members on the day coverage took effect.
Social security numbers. -Effective
on enactment, the amendments make it a misdemeanor (1) to willfully,
knowingly, and with intent to deceive the Secretary of Health, Education,
and Welfare as to someone's identity, furnish false information
to the Secretary in connection with the establishment and maintenance
of social security records and (2) to use a social security number
obtained on the basis of false information, to falsely represent
a number to be a social security number, or to use someone else's
social security number, for the purpose of increasing a payment
under social security or any other federally funded program, or
for the purpose of obtaining such payment.
The provision directs the Secretary to issue
social security numbers to (1) aliens at the time of their adinission
for permanent residence and aliens at the time they are admitted
temporarily with permission to work or at the time their status
is changed to permit them to work; (2) any individual who applies
for or receives benefits under any Federal or federally subsidized
program, and (3) any individual who could have been but was not
assigned a number under the categories listed above.
The Secretary is authorized, but not directed
to issue social security numbers to schoolchildren and to preschool
children upon request by the parents or guardians. In addition,
the Secretary is required to establish the age, citizenship, alien
status, and identity of all applicants for social security numbers.
Medicare
Medicare for the disabled. -Medicare
protection is extended to persons entitled for not less than 24
consecutive months to cash benefits under the social security and
railroad retirement programs because they are disabled. Coverage
includes disabled workers at any age, disabled widows, and disabled
dependent widowers between ages 50 and 65; women aged 50 or older
who are entitled to mother's benefits and, for 24 months
before the first month they would have been entitled to Medicare
protection, met all the requirements for disability benefits except
for actual filing of a disability claim; those aged 18 and over
who receive social security benefits because they became disabled
before reaching age 22; and disabled qualified railroad retirement
annuitants. Medicare protection under this provision will begin
with the later of (a) July 1973 and (b) the 25th consecutive month
of an individual's entitlement to social security disability benefits
and will terminate the month following the month notice of termination
of disability benefits is mailed.
Chronic kidney disease deemed to constitute
a disability for purposes of Medicare.-Effective July 1, 1973,
Medicare coverage is extended to individuals under age 65 who are
currently or fully insured or entitled to monthly social security
benefits, and to the spouses and dependent children of such individuals,
who require hemodialysis or renal transplantation for chronic renal
disease. Such individuals are deemed to be disabled for purposes
of coverage under both parts of Medicare. Eligibility for coverage
begins with the third month after the month in which a course of
renal hemodialysis begins through the twelfth month after the month
in which an individual had a transplant or dialysis terminates.
Benefits include those of both parts of Medicare, with the usual
deductibles and coinsurance. The, Secretary is authorized to limit
reimbursement for treatment to kidney disease treatment centers
that meet regulatory requirements. These requirements include a
minimal utilization rate for covered procedures and a medical review
board to screen patients for medical suitability for treatment.
Health Maintenance Organization option.-Individuals
eligible for both parts of Medicare, or for SMI only, may choose
to have their covered care provided through a health maintenance
organization (HMO)--a prepaid group health or other capitation plan
that meets prescribed standards. Two methods of reimbursement for
HMO's are to be established. Under the first, an HMO will be "at
risk" and payments will be made on an incentive capitation
basis. This method, which can be used only by substantial, established
HMO's, will permit the HMO and the Government to share, according
to a prescribed formula, in any savings the HMO achieves
in relation to adjusted average per capita costs of covered health
services for persons outside the HMO. The second method, which must
be used by newly established HMO's and may be used by any other
HMO, provides for interim monthly capitation payments subject to
year-end adjustment that reflects the HMO's actual reasonable costs
of providing Medica re- covered services.
A beneficiary enrolled with an established
HMO that uses the risk-sharing method of reimbursement will receive
covered services only through the HMO, except for emergency services
and urgently needed services received when he is temporarily outside
the HMO's service area. A beneficiary enrolled in an HMO receiving
cost reimbursement will not be required to use the HMO as his single
source of health care. Payment will be made by Medicare in the usual
manner for services he receives outside the HMO.
The provision is effective with respect to
services provided on or after July 1, 1973.
Professional Standards Review Organizations.
- By January 1, 1974, the Secretary must establish areas throughout
the United States with respect to which Professional Standards Review
Organizations (PSRO's) may be designated. They are to consist of
substantial numbers of practicing physicians (usually 300 or more)
in a local area and will be responsible for comprehensive and ongoing
review of services covered under the Medicare, Medicaid, and maternal
and child health care programs. They are to assure that services
are (1) medically necessary and (2) provided in accordance with
professional standards. The PSRO's are not required to review services
other than institutional care and services unless they so choose
and the Secretary agrees. They will not be involved with reasonable
charge determinations; they are required to recognize and use
utilization review committees in hospitals and other medical
organizations to the extent these are deemed effective by the PSRO.
Safeguards, designed to protect the public interest and to prevent
pro forma carrying out of review responsibilities, include
appeals procedures.
Until January 1, 1976, the Secretary will
be able to make an agreement only with a qualified organization
representing a substantial proportion of the physicians in the designated
geographical area. Until January 1, 1976, the Secretary
is also required to poll the practicing physicians in the
area--at the request of 10 percent or more of such physicians--to
determine whether or not an organization of physicians that has
requested an agreement with the Secretary to establish a PSRO substantially
represents the area's practicing physicians. If more than 50 percent
of the practicing physicians responding to the poll indicate that
the organization does not substantially represent them, the Secretary
cannot enter into an agreement with that organization.
Level-of-care requirements in skilled
nursing facilities.-The Medicare definition of covered extended-care
services is broadened somewhat, and the same definition applies
to skilled nursing facility services under Medicaid. Services covered
are those provided directly by or requiring the supervision of skilled
nursing personnel, or skilled rehabilitation services needed by
the patient on a daily basis that, as a practical matter, can only
be provided in a skilled nursing facility on an inpatient basis.
Medicare coverage will also continue during short periods when no
skilled services were actually provided but when discharge from
a skilled facility for such brief period is neither desirable nor
practical. This provision is applicable to services furnished after
December 31, 1972.
Waiver of beneficiary liability in certain
situations where Medicare claims are disallowed. Medicare beneficiaries
will be "held harmless" in certain situations where claims
are disallowed but the beneficiary is without fault, including cases
where the disallowance is based on determinations that the services
were not medically necessary or did not meet level-of-care requirements.
Where the beneficiary is "held harmless," liability shifts
either to Medicare or, where it is found that the provider has not
acted with due care, to the provider. This provision is applicable
to claims for services provided after the date of enactment.
Advance approval of extended-care and
home health coverage.-The Secretary is authorized to establish,
by medical condition, specified periods of time after hospitalization
during which a patient will be presumed to require an extended care
level of services. Where a patient's physician certifies to the
need for such care and submits to the extended-care facility, in
advance of admission, a plan for carrying out the services, the
care furnished will be assumed to be the type of care covered as
extended care. Comparable provisions applying to post-hospital home
health services are also included. The advance approval provision
can, however, be declared inapplicable to patients of any physician
who is found to be unreliable in certifying patients' need for such
care. In addition, an extended-care facility's utilization review
committee can terminate payment to a patient during the approved
period if it determines that further inpatient stay is no longer
medically necessary. The provision specifically restricts to retroactive
application of regulations pertinent to the provision. This provision
is effective for admissions for extended-care services or the initiation
of home health plans on or after January 1, 1973.
Hospital insurance for the uninsured.-Persons
reaching age 65 who are ineligible for hospital insurance may enroll,
on a voluntary basis, for such coverage under the same conditions
as for supplementary medical insurance. Those who enroll will pay
the full cost of the protection--$33 a month at the beginning and
more in later years as hospital costs rise; enrollment for supplementary
medical insurance is also required. States and public organizations,
through agreements with the Secretary, are permitted to purchase
such protection on a group basis for their aged retired (or active)
employees. Coverage under this provision will be effective on July
1, 1973.
Medicare services outside the United
States- Inpatient hospital services furnished a resident of
the United States in a foreign hospital that is closer or substantially
more accessible to his residence than the nearest suitable United
States hospital will be covered. Payments under SMI for necessary
physicians' and ambulance services furnished in connection with
such hospitalization is also authorized, whether or not an emergency
exists. Medicare payments are also authorized for emergency inpatient
hospital services and related physicians' services needed by beneficiaries
traveling in Canada between Alaska and another State. This provision
applies to hospital admissions after December 31, 1972.
Elimination of provisions preventing
enrollment under SMI more than 3 years after first opportunity-
Eligible persons may enroll under SMI during any prescribed enrollment
period. Beneficiaries are no longer required to enroll within 3
years following first eligibility or a previous withdrawal from
the program. The requirement that the SMI premium for late enrollees
be increased 10 percent for each 12 months elapsing between the
time they could have enrolled and actually do enroll is retained.
This provision is effective on enactment.
It applies to all those ineligible to enroll because of the 3-year
limit in effect under the old law.
Coordination between Medicare and Federal
employees' plans.- Effective January 1, 1975, no payment will
be made under Medicare for the same services covered under a Federal
employees health benefits (FEHB) plan unless in the meantime the
Secretary certifies that such plan or the FEHB program has been
modified to make available coverage supplementary to Medicare benefits
and that Federal employees and retirees will continue to have the
benefit of a contribution toward their health insurance premiums
from either the government or the individual plan.
Uniform Medicare and Medicaid standards
for nursing facilities.- A single "skilled nursing facility"
definition is established, as well as a single health, safety, environmental,
and staffing standards for institutions formerly identified as extended-care
facilities under Medicare and nursing homes under Medicaid. In the
future, extended-care services covered under Medicare will be provided
in institutions identified as "skilled nursing facilities"
rather than as "extended-care facilities." Under both
Medicare and Medicaid, a "skilled nursing facility" must
meet the existing statutory conditions of participation for extended-care
facilities plus certain additional requirements that skilled nursing
homes must meet under existing Medicaid law. Where a skilled nursing
facility desires to participate in Medicare and Medicaid, the Secretary's
determination that it meets Medicare standards would also serve
for Medicaid. Uniformity of standards will be effective July 1,
1973.
Reimbursement rates for skilled nursing
facilities and intermediate-care facilities. -States will
be required to develop methods for reimbursing skilled
nursing facilities and intermediate -care facilities on a basis
reasonably related to cost and to implement these methods under
Medicaid (after approval by the Secretary) by July 1, 1976. These
State payment rates for skilled nursing facilities can then be used
under Medicare in reimbursing for extended-care services. The Medicaid
rates can be adjusted upward, but not more than 10 percent, to account
for specific factors related to Medicare not included by the State
in computing Medicaid rates.
14-day-transfer requirement for post-hospital
extended-care benefits.-The Medicare extended-care benefit
requirement that a patient's transfer to an extended-care facility
take place within 14 days of his discharge from a hospital is modified
to permit a longer interval for patients whose conditions do not
permit provision of skilled services within 14 days (for example,
a patient whose hip fracture has not mended to
the point that physical therapy and restorative
nursing can be utilized). An extension, not to exceed 2 weeks beyond
the original 14- days, is authorized also in instances where admission
to a facility providing extended-care services is prevented because
of a shortage of appropriate bed-space in a geographic area.
Medical social services.-The Secretary
may no longer require the provision of medical social services as
a condition of participation for skilled nursing facilities under
Medicare and Medicaid.
Waiver of registered-nurse requirement
in skilled nursing facilities in rural areas.-The Secretary
may waive the requirement that a skilled nursing facility must employ
a registered nurse full time (to the extent that "full time"
is deemed to mean more than 40 hours a week) for certain rural skilled
nursing facilities unable to assure the presence of a full-time
registered nurse 7 days a week. A facility of this type that has
one full time registered nurse and is making good-faith efforts
to obtain another will be allowed a special waiver of the nursing
requirement with respect to not more than two day shifts--over a
weekend, for example. This special waiver will be authorized if
the facility has only patients whose physicians have indicated that
the individual can be without a registered nurse's services for
a 48-hour period. If the facility has any patients for whom physicians
have indicated a need for daily skilled nursing services,
it must make arrangements for a registered nurse or a physician
to spend enough time at the facility to provide the skilled services
needed.
Amount of supplementary medical insurance
premium.-The Secretary will continue to determine and promulgate
in December 1972 and each year thereafter a monthly enrollee
premium (applicable for both the aged and the disabled) for the
following fiscal year. The enrollee premium will, however, be increased
only in the event of a general benefit increase--either an automatic
increase or one resulting from future legislation. In any given
year, the premium will rise by no more than the percentage by which
cash benefits have been increased across the board since the premium
was last increased. Federal general revenues will finance that part
of program costs not met through enrollee premiums.
The change is effective for the fiscal year
beginning July 1973. (Through June 1973, the premium amount is $5.80,
and it will be $6.30 through July 1974.)
Change in SMI deductible.-The SMI
deductible is increased from $50 to $60 as of January 1, 1973.
Elimination of coinsurance payment with
respect to home health services under SMI.-Payments for home
health services furnished under SMI are to be in
amounts equal to 100 percent of the reasonable cost of services,
rather than 80 percent as in the old law.
Automatic enrollment for SMI- Aged
and disabled beneficiaries, except for residents of Puerto Rico
and foreign countries, will be automatically enrolled for SMI as
they become entitled to hospital insurance. Persons eligible for
automatic enrollment, will, to the extent possible, be fully informed
and given an opportunity to decline the coverage. This provision
applies to any individual whose initial enrollment period begins
after March 31, 1973, or who becomes entitled to hospital insurance
after June 1973.
Coverage of chiropractors' services-
Coverage is provided for the services of licensed chiropractors
who also meet uniform minimum standards, but only with respect to
treatment by means of manual manipulation of the spine and only
with respect to correction of subluxation of the spine demonstrated
by X-ray. This provision will be effective July 1, 1973.
Limitation on Federal participation for
capital expenditures.- The Secretary may withhold
or reduce reimbursement amounts to providers of services
under title XVIII for depreciation, interest, and, in the case of
proprietary providers, a return on equity capital, or other expenses
related to capital expenditures for plant and equipment in excess
of $100,000, which are determined to be inconsistent with State
or local health facility plans. The Secretary will act on the basis
of findings and recommendations submitted to him by various health
facility planning agencies. If, after consultation with an appropriate
national advisory council, the Secretary determines that a disallowance
of expenses will discourage the operation or expansion of an organization
that has demonstrated capability of economically providing comprehensive
health care services or would otherwise be inconsistent with effective
organization and delivery of health services or effective administration
of titles V, XVIII, or XIX, he is authorized to
allow such expenses. This provision is effective with respect to
obligations for capital expenditures incurred after December 31,
1972, or earlier, if a State so requests.
Experiments and demonstration projects
in prospective reimbursement and incentives for economy.- The
Secretary is authorized to test various methods of making
payment to providers of services on a prospective basis under the
Medicare, Medicaid, and maternal and child health programs. In addition,
he is authorized to conduct experiments with methods of payment
or reimbursement designed to increase efficiency and economy (including
payment for services furnished by organizations providing comprehensive,
mental, or ambulatory health care services as well as ambulatory
surgical centers); with performance incentives for intermediaries
and carriers; with reimbursement implications of paying for services
rendered by physicians' assistants with the use of intermediate
care and homemaker services by beneficiaries who either are ready
for discharge from a hospital or are unable to maintain themselves
at home without assistance; and with programs designed to improve
the rehabilitation of patients in long-term health care facilities.
The Secretary is also authorized to determine whether services of
clinical psychologists might be made more generally available to
persons eligible under Medicare and Medicaid.
Limitations on recognition of increase
in prevailing charge levels for medical and other health services.-
To determine the reasonableness of charges by physicians under Medicare,
Medicaid, and maternal and child health programs: (a) after December
31, 1970, medical charge levels recognized as prevailing may not
be increased beyond the 75th percentile of actual charges in a locality
during the calendar year elapsing before the start of the fiscal
year; (b) for fiscal year 1974 and thereafter, the prevailing charge
levels recognized for a locality may be increased, in the aggregate,
only to the extent justified by indexes reflecting changes in costs
of practice of physicians and in earnings levels; and (c) for medical
supplies, equipment, and services that, in the judgment of the Secretary,
generally do not vary significantly in quality from one supplier
to another, charges allowed as reasonable after December 1972 may
not exceed the lowest levels at which the supplies, equipment, and
services are widely and consistently available in a locality. The
existing Health Insurance Benefits Advisory Council, which has been
engaged in a study of the methods of reimbursement of physicians'
under Medicare, is to report its findings to the Congress.
Financing
Consistent with past policy of maintaining
the security program on a sound financial basis, provision is made
for meeting the cost of the expanded program. The costs of the cash
benefits program and the hospital insurance program are financed
by revised contribution rate schedules. For 1973, the combined contribution
rate for benefits and hospital insurance is increased from the previously
scheduled 5.5 percent each for employers and employees to 5.85 percent
each. The provisions relating to the earnings base for tax and benefit
purposes in the law (as amended in July 1972) are retained: the
maximums of $10,800 for 1973 and of $12,000 for 1974, with automatic
increases thereafter as wages rise. The cost estimates underlying
the contribution rates were based on the new financing principles
adopted earlier in 1972 under Public Law 92-336. The schedules for
contribution rates under the provisions now in the law and under
the previous provisions are shown in the accompanying table.
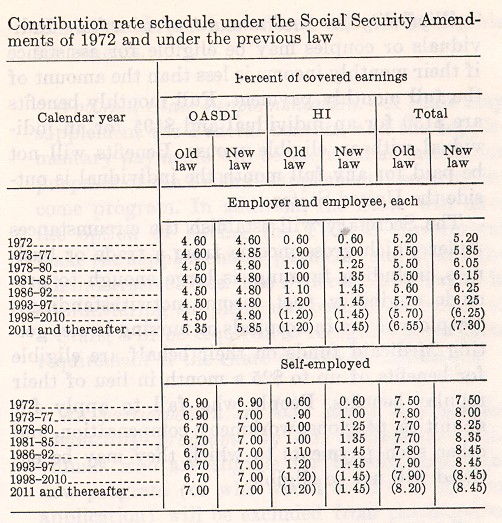
Supplemental Security Income for the Aged, Blind, and Disabled
The existing Federal-State programs of aid
to the aged, blind, and permanently and totally disabled are repealed,
effective January 1, 1974 (except in Puerto Rico, the Virgin Islands,
and Guam), and a new, totally Federal supplemental security income
program will become effective on that date. The new national program,
designed to provide financial assistance to needy people who have
reached age 65 or are blind or disabled is established by amendment
of title XVI of the Social Security Act. The program
is to be administered by the Social Security Administration.
Eligibility for and amount of beneflts.-Individuals
or couples may be eligible for assistance if their monthly income
is less than the amount of the full monthly payment. Full monthly
benefits are $130 for an individual and $195 for an individual with
an eligible spouse. Benefits will not be paid for any full month
the individual is outside the United States.
The Secretary will establish the circumstances
under which gross income from a trade or business, including farming,
is large enough to preclude eligibility (net income notwithstanding).
People who are in hospitals or nursing homes getting Medicaid funds
on their behalf are eligible for benefits of up to $25 a month in
lieu of their regular benefits. People who fail to apply for annuities,
pensions, workmen's compensation, and other such payments to which
they may be entitled will not be eligible.
Income as defined by the program.-In
determining an individual's eligibility and the amount of his benefits,
both his earned and unearned income are taken into consideration.
The definition of earned income follows generally the definition
of earnings used in applying the retirement test under the social
security program. Unearned income means all other forms of income,
including benefits from other public and private programs, prizes
and awards, proceeds of life insurance not needed for expenses of
last illness and burial (with a maximum of $1,500), gifts, inheritances,
rents, dividends, interest, and so forth. For people who live as
members of another person's household, the value of their room and
board will be deeined to be one-third of the full monthly payment.
These items are to be excluded from income:
(1) $20 of any income (earned or unearned)
other than income paid on the basis of need;
(2) $65 of earnings a month and one-half
above that (plus income necessary for fulfilling plans for self-support
for the blind and disabled and work expenses for the blind) ;
(3) within reasonable limits, earnings of
a student regularly attending school;
(4) an individual's irregular and infrequent
earned income of $30 or less in a quarter and irregular and infrequent
unearned income of $60 or less in a quarter;
(5) any amount received from a public agency
as a refund of taxes paid on real property or on food purchased;
(6) the tuition and fees part of scholarships
and fellowships;
(7) home produce;
(8) one-third of child-support payments from
absent parent;
(9) foster care payments for a child placed
in the household by a child-placement agency; and
(10) supplementary benefits based on need
and provided by a State or political subdivision.
Exclusions from resources.-Generally, individuals will
not be eligible for payments if they have resources in excess of
$1,500 and couples will not be eligible if their resources are above
$2,250. Those who were receiving aid to the aged, blind and disabled
in December 1973 under an approved State plan, but whose resources
were greater than those permitted under the Federal program, will
be considered not to have exceeded this amount until the resources
do not exceed the maximum amounts permitted under the State plan
in effect for October 1972. The following will be excluded from
resources:
(1) The home and appurtenant land to the
extent that their value does not exceed a reasonable amount;
(2) household goods, personal effects, and
an automobile, not in excess of a reasonable amount;
(3) other property essential to the individual's
support (within reasonable value limitations);
(4) life insurance policies, if their total
face value is $1,500 or less--otherwise, insurance policies would
be counted only to the extent of their cash surrender value;
(5) resources of a blind or disabled individual
necessary for fulfilling an approved plan of self support; and
(6) shares of certain nonnegotiable stock
held in a Regional or Village Corporation by Alaskan natives.
The Secretary will prescribe time limits and ways of disposing of
excess property so that it will not be included as resources.
Definitions of terms.-The terms
used in the SSI program in a particular sense are defined below.
An eligible individual: A resident
of the United States and a citizen or an alien admitted for permanent
residence or otherwise permanently re siding in the United States
under color of law, and aged, blind, or disabled.
Aged individual: One aged 65 or
older.
Blind individual: An individual
who has central visual acuity of 20/200 or less in the better eye
with the use of a correcting lens, or equivalent impairment in the
fields of vision.
Disabled individual: An individual
who is unable to engage in substantial gainful activity by reason
of a medically determinable physical or mental impairment that is
expected to last or has lasted for 12 months or can be expected
to result in death. (This definition is the same as that used for
social security disability benefits.) A child under age 18 who is
not engaging in substantial gainful activity will be considered
disabled if he suffers from any medically determinable physical
or mental impairment of comparable severity. A disabled individual
will be entitled to a 9-month trial work period unless he has had
a prior trial work period during a period of eligibility based on
the same disability. A disabled individual who is medically determined
to be an alcoholic or drug addict will not be entitled to benefits
under this program unless he undergoes appropriate available treatment
in an approved facility.
(Those blind or disabled individuals who
are on the benefit rolls in December 1973 under existing State programs
will be considered blind or disabled for purposes of this program
if they met the definition of disability or blindness which was
in effect as of October 1972.)
Eligible spouse: An aged, blind,
or disabled individual who is the husband or wife of an individual
who is aged, blind, or disabled and who has not been living apart
from such other spouse for more than 6 months.
Child: An unmarried person who is
not the head of a household and who is either under the age of 18
or under the age of 22 and attending school regularly.
Determination of marital relationship:
Appropriate State law will apply except that when two persons,
for purposes of receiving social security benefits, are considered
married and when two persons hold themselves out as married in the
community in which they live, they will be considered married for
purposes of this program.
The Income and resources of a spouse living
with an eligible individual will be taken into account in determining
the benefit amount of the individual, whether or not the income
and resources are available to him. Income and resources of a parent
may count as income of a disabled or blind child.
Rehabilitation Services.-Disabled
and blind beneficiaries will be referred to State agencies for vocational
rehabilitation services. A beneficiary who refuses without good
cause any vocational rehabilitation services offered will not be
eligible for benefits.
Optional State supplementation.-A
State may supplement the Federal benefits, and the supplementary
payments will be excluded as income for purposes of the Federal
supplemental security income program. In addition, the State will
have the option of having the Federal Government make the supplementary
payments and absorb the administrative costs. The Federal Government,
in administering supplemental benefits on behalf of a State, will
be required to recognize a residence requirement if the State decides
to impose one.
No participation in food stamp and surplus
commodity programs by SSI recipients.-Individuals who are eligible
for benefits under the new program (or who would be if they filed
an application) will be excluded from participation in food stamp
and surplus commodity programs.
Determination of Medicaid eligibility.-The
Secretary may enter into agreements with States under which he will
determine eligibility for medical assistance for aged, blind, and
disabled persons under title XIX. The State would pay half of the
Secretary's additional administrative costs arising from carrying
out the agreement.
Limitations on increases in State welfare
expenditures.-States are guaranteed that, if they provide payments
that supplement the Federal SSI program and that are administered
by the Federal Government, it will cost them no more to do so than
the amount of their total expenditures for cash public assistance
payments to the aged, blind, or disabled during calendar year 1972--that
is, to the extent that the Federal payments and the State supplementary
payments do not exceed the payment levels in effect under the public
assistance programs in the State for January 1972, plus the value
of food stamps if the State pays in cash the value of food stamps.
|